For years, scientists have sought to understand the origins of autism spectrum disorder (ASD), a complex neurodevelopmental condition. While genetics and environmental factors have been extensively studied, recent research suggests that the maternal gut microbiome during pregnancy may play a pivotal role in influencing the risk of ASD in offspring.
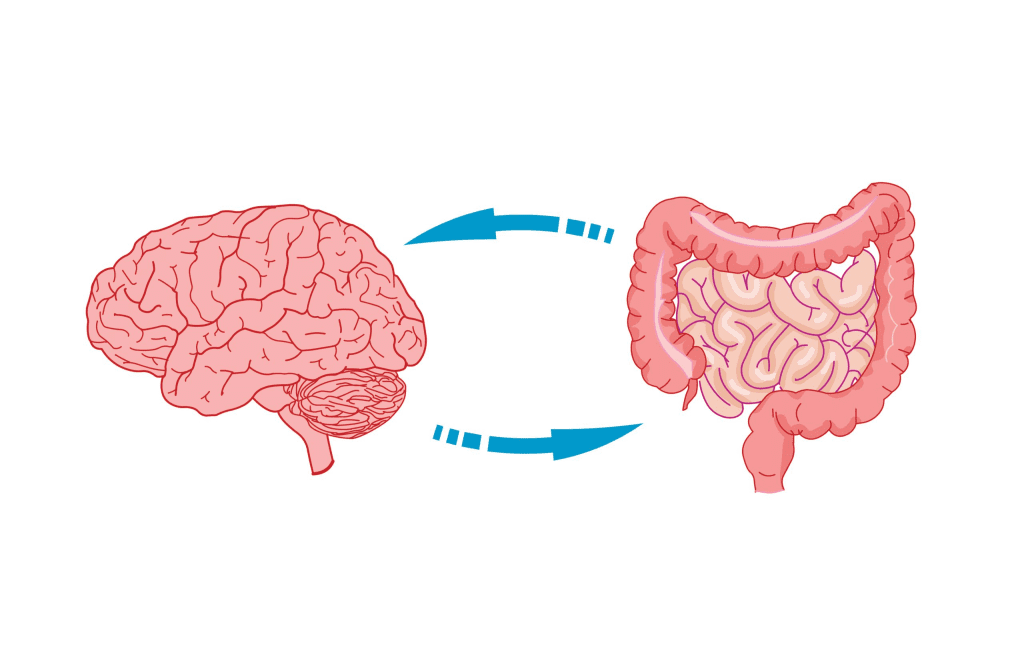
The Gut-Brain Connection: A Deeper Insight
The gut-brain axis has long been recognized as a critical pathway through which the gastrointestinal tract communicates with the central nervous system. This connection influences various aspects of health, including mood, immune function, and neurological development. Emerging evidence indicates that the maternal gut microbiome—the community of microorganisms residing in the digestive tract—may significantly impact fetal brain development.
The Role of IL-17a in Neurodevelopment
A groundbreaking study conducted by researchers at the University of Virginia School of Medicine has shed light on the potential mechanisms linking the maternal microbiome to ASD. The study focused on interleukin-17a (IL-17a), an immune molecule known for its role in inflammatory responses. Using mouse models, the researchers demonstrated that maternal immune activation leading to increased IL-17a levels during pregnancy resulted in offspring exhibiting autism-like behaviors, such as social deficits and repetitive actions. Notably, when IL-17a was inhibited, these behavioral abnormalities were prevented, underscoring its critical role in neurodevelopment.
Microbiome Transplantation and Behavioral Outcomes
To further explore the influence of the maternal microbiome, the researchers conducted fecal microbiota transplantation experiments. They transferred gut bacteria from mice with pro-inflammatory microbiota to those with a non-inflammatory profile. The recipient mice, upon pregnancy, produced offspring that also exhibited autism-like behaviors, despite having different genetic backgrounds. This finding emphasizes that the composition of the maternal gut microbiome, rather than genetics alone, can significantly affect neurodevelopmental outcomes in offspring.
Implications for Human Health
While these findings are based on animal models, they open new avenues for understanding the etiology of ASD in humans. If similar mechanisms are confirmed in human studies, it could revolutionize prenatal care by highlighting the importance of maintaining a healthy maternal microbiome during pregnancy. Potential interventions might include dietary modifications, probiotic supplementation, or other strategies aimed at promoting a balanced gut microbiota to support optimal fetal brain development.
A Multifaceted Approach to Autism Research
This research adds to the growing body of evidence suggesting that ASD arises from a complex interplay of genetic, environmental, and immunological factors. Other studies have identified genetic mutations, such as those in the DDX53 gene, and environmental exposures, like air pollution, as contributors to ASD risk. The integration of these diverse findings underscores the need for a comprehensive, multidisciplinary approach to autism research and prevention.
Looking Ahead
The discovery of the maternal microbiome’s influence on neurodevelopment represents a significant step forward in unraveling the complexities of ASD. Future research will be essential to validate these findings in human populations and to develop targeted interventions that can mitigate ASD risk. As our understanding of the gut-brain axis deepens, it holds promise for informing strategies that support maternal and child health, potentially reducing the incidence of neurodevelopmental disorders like autism.
Note: This article is based on current scientific research and is intended for informational purposes. Individuals should consult healthcare professionals for personalized medical advice.





